Platelet-activating factor (PAF) is a potent mediator of inflammation. PAF has a number of biologic effects of relevance in asthma. The inflammatory response in asthma, such as eosinophils, mast cells, macrophages, neutrophils, and platelets are involved in PAF. PAF causes bronchoconstriction, microvascular leakage, mucus hypersecretion, and an increase in bronchial hyperresponsiveness (BHR) in animal models. In a word, PAF is an important mediator in asthma. However, in this study, Modipafant is a potent, selective PAF antagonist. It is the enantiomer possessing most of the activity present in the racemate UK-74505. Modipafant has no effect on antigen challenge. Thus, the active (+)-enantiomer Modipafant has no effect in chronic asthma. PAF is not an important mediator in asthma. In addition, potent and selective antagonists of PAF are of interest as a tool to investigate the role of PAF in the various pathophysiological conditions.
In preincubated with rabbit platelets, the potency of antagonizing PAF induced aggregation increases markedly when preincubation time with Modipafant. It increases from 2 min (IC50=5.6 nM) to 60 min (IC50=0.34 nM).
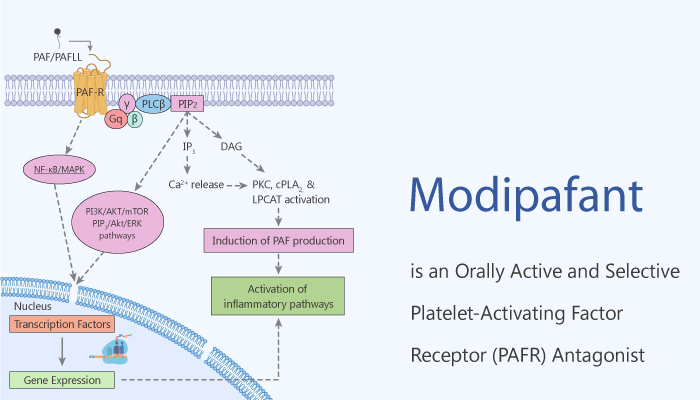
In summary, PAF has multiple actions that could make it a potential mediator in asthma, but not important. PAF is capable of recruiting and activating inflammatory cells, causing the secondary release of leukotrienes, prostaglandins, and oxygen-free radicals. In addition, It is a bronchoconstrictor, can increase bronchial mucus secretion, and cause microvascular leakage. Modipafant is a potent, orally active, and selective PAF antagonist. It exhibits approximately double the intrinsic potency of UK-74505, and It is a useful tool to investigate the role of PAF in various pathophysiological conditions.
Reference:
Kuitert LM, et al. Am J Respir Crit Care Med. 1995;151(5):1331-1335.