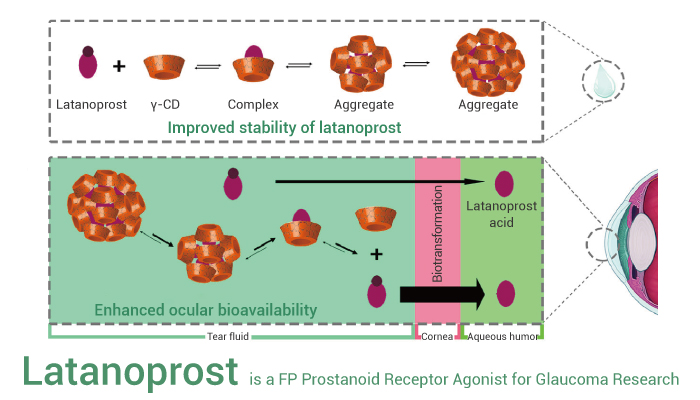
Glaucoma, a prevalent disease of the eye, involves the degeneration of the optic nerve and eventually leads to irreversible neurodegenerative blindness. Usually, the disturbance of aqueous humor discharge is a major cause of glaucoma. Besides, the intraocular pressure (IOP) increases in glaucoma. Therefore, reducing IOP is an effective intervention method to reduce the occurrence of glaucoma. Latanoprost (PHXA41) is a prostaglandins F2α (PGF2α) analogue, and can be used for glaucoma research. Specifically, It can effectively pass through cornea and then the esterase can hydrolyze it to latanoprost acid. Moreover, latanoprost acid is an F-prostaglandin (FP) receptor agonist, and can effectively reduce intraocular pressure (IOP) by increasing the outflow of aqueous humor through uvea. In addition, Latanoprost also has ocular hypotensive and neuroprotective effects.
Latanoprost, a F-prostaglandin prostanoid receptor agonist, can be used for glaucoma research.
In vitro, Latanoprost (0.1 μΜ, 24 h) significantly increases cell viability, promotes neurite outgrowth, and increases the levels of p-Akt and p-mTOR expression in RGC-5 cells. However, this effect is blocked by the FP receptor inhibitor AL8810 (10 μM). The result indicates that Latanoprost promotes neurite outgrowth through an FP receptor-mediated modulation of the PI3K-Akt-mTOR signaling pathway. Furthermore, Latanoprost (0.03 or 0.3 μg/mL) increases MMP-9 activity by 75% and 75%, respectively, in human CBSM cells.
In vivo, a single drop of Latanoprost (0.005%, applied topically) results in marked miosis, anterior bowing of the peripheral iris, narrowing of the iridocorneal angle, and shallowing of the anterior chamber of the beagle dog. Moreover, following Latanoprost, the pupil diameter, ACA, and AOD decreases 84%, 14%, and 16%, respectively.
In conclusion, Latanoprost, a prostaglandins F2α analogue, has antiglaucoma, ocular hypotensive and neuroprotective effects.
References:
[1] Zhou X, et al. Eur J Pharm Sci. 2021 May 1;160:105758.
[2] Zheng J, et al. Cell Mol Neurobiol. 2011 May;31(4):597-604.
[3] Ooi YH, et al. Invest Ophthalmol Vis Sci. 2009 Nov;50(11):5259-65.