Adrenergic receptors are a class of G protein-coupled receptors that are targets of the catecholamines, especially norepinephrine and epinephrine. Many cells possess these receptors, and the binding of a catecholamine to the receptor will generally stimulate the sympathetic nervous system. The sympathetic nervous system is responsible for the fight-or-flight response, which includes widening the pupils of the eye, mobilizing energy, and diverting blood flow from non-essential organs to skeletal muscle. There are two main groups of adrenergic receptors, α and β, with several subtypes. α receptors have the subtypes α1 and α2. β receptors have the subtypes β1, β2 and β3. All three are linked to Gs proteins, which in turn are linked to adenylate cyclase. Agonist binding thus causes a rise in the intracellular concentration of the second messenger cAMP.
Mirabegron is a Selective β3-adrenoceptor Agonist for Overactive Bladder Research
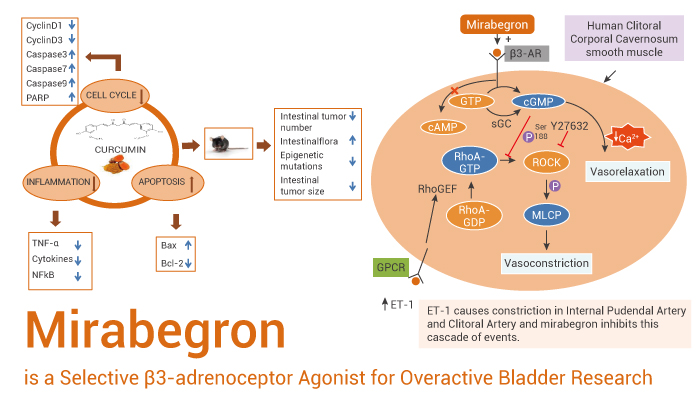
Mirabegron is a selective β3-adrenoceptor agonist with an EC50 value of 22.4 nM.
In Vitro, Mirabegron (YM178) increases cyclic AMP accumulation in Chinese hamster ovary (CHO) cells expressing human β3-adrenoceptor (AR). EC50 value is 22.4 nM. EC50 values of Mirabegron for human β1– and β2-ARs are 10,000 nM or more, respectively. EC50 of Mirabegron in rat bladder strips precontracted with 10-6 M Carbachol (CCh) is 5.1 μM. Whereas that in human bladder strips precontracted with 10-7 M CCh is 0.78 μM. And it concentration-dependently increases the accumulation of cAMP in CHO cells expressing human β3-ARs, with an EC50 value of 22.4 nM.
In Vivo, Mirabegron (YM178) produces a dose-dependent decrease in the frequency of rhythmic bladder contraction in anesthetized rats. In contrast, Mirabegron does not decrease the amplitude of rhythmic bladder contraction at up to 3 mg/kg i.v.. On the contrary, Oxybutynin (0.272 mg/kg; i.v.) significantly increases the frequency of rhythmic bladder contraction and decreased its amplitude.
In conclusion, Mirabegron is a selective β3-adrenoceptor agonist for overactive bladder research.
Reference:
[1]. J Pharmacol Exp Ther. 2007 May;321(2):642-7.