Neprilysin (NEP) is a neutral endopeptidase. Neprilysin inhibitors increase the levels of atrial natriuretic peptides, therefore have beneficial effects for the cardiovascular diseases, including hypertension and heart failure. In addition, angiotensin receptors are a class of G protein-coupled receptors with angiotensin II as their ligands. They are responsible for the signal transduction of the vasoconstricting stimulus of the main effector hormone, angiotensin II.
A dual-acting angiotensin receptor-neprilysin inhibitor (ARNi), which would not directly affect ACE or APP activity, may therefore be a safer approach to inhibit the RAAS and increase natriuretic peptide levels.
Sacubitril/Valsartan (LCZ696) is a first-in-class, orally active, and dual-acting angiotensin receptor-neprilysin (ARN) inhibitor.
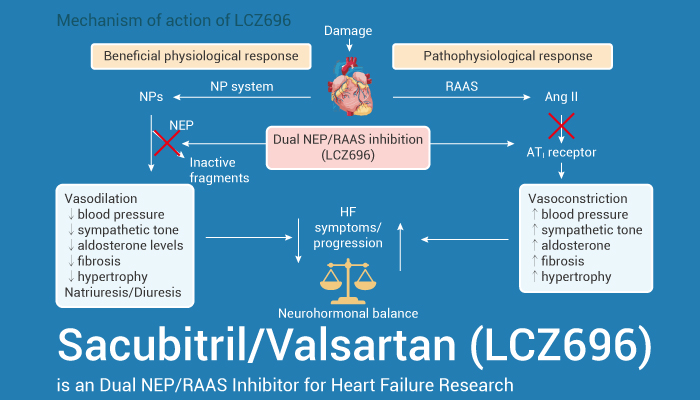
In addition, Sacubitril/Valsartan inhibits the excessive activation of the renin-angiotensin-aldosterone system (RAAS) while simultaneously increasing the cardiovascular protection provided by the natriuretic peptide system. Importantly, Sacubitril/Valsartan has the potential for hypertension and heart failure research. For example, Sacubitril/Valsartan (oral administration) causes dose-dependent increases in atrial natriuretic peptide immunoreactivity in Sprague-Dawley rats. Then it provides sustained, dose-dependent blood pressure reductions in hypertensive double-transgenic rats. Besides, Sacubitril/Valsartan improves heart function effectively in streptozotocin (STZ)-induced diabetic mice and to reduce fibrosis by inhibiting TGF-β during heart failure. In vitro, in H9C2 cardiomyoblast cells under high-glucose (HG) conditions, Sacubitril/Valsartan inhibits the nuclear transfer of NF-κB and JNK/p38MAPK phosphorylation. Furthermore, Sacubitril/Valsartan mitigates inflammation and apoptosis in H9C2 cardiomyocytes.
In summary, Sacubitril/Valsartan is an orally active angiotensin receptor-neprilysin (ARN) inhibitor, has the potential for hypertension and heart failure research.
References:
[1] Jessie Gu, et al. J Clin Pharmacol. 2010 Apr;50(4):401-14.
[2] Qing Ge, et al. Exp Biol Med (Maywood). 2019 Sep;244(12):1028-1039.