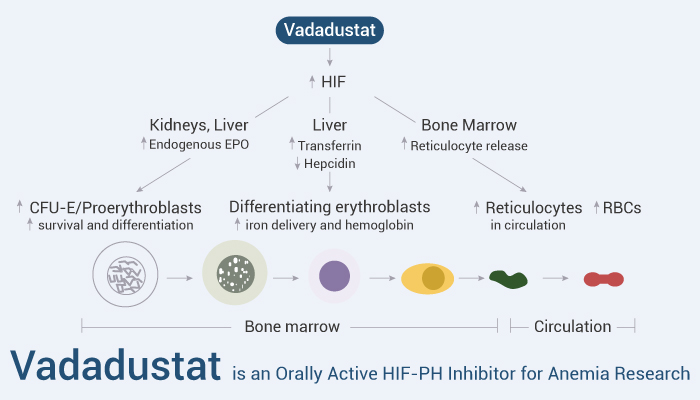
Chronic kidney disease (CKD) develop anemia largely because of inappropriately low erythropoietin (EPO) production and insufficient iron available to erythroid precursors. EPO production is controlled by hypoxia‐inducible factor (HIF). HIF is a multicomponent transcription factor. It is mainly regulated by the degradation rate of one of its components, HIFα. HIFα is targeted for polyubiquitination and proteasomal degradation by prolyl hydroxylation. Three specific HIF prolyl hydroxylases (HIF prolyl‐4‐hydroxylase domain [HIF‐PHD] enzymes) use oxygen, 2‐oxoglutarate, and one of three HIFα proteins (HIF‐1α, HIF‐2α, or HIF‐3α) as substrates.
Vadadustat is an investigational oral HIF‐PH inhibitor. It stabilizes intracellular HIFα, increases serum EPO concentrations over baseline in healthy individuals and in patients with CKD.
On March 27, 2024, FDA approved vadadustat for the treatment of anemia caused by chronic kidney disease
Here we will introduce the Vadadustat effects on erythropoiesis.
Firstly, Vadadustat pharmacologically increases hypoxia‐inducible factor (HIF) and transcription of HIF target genes. In the kidneys and liver, vadadustat improves production of endogenous erythropoietin (EPO). Secondly, EPO increases survival and differentiation of marrow erythroid progenitors (colony‐forming units erythroid/proerythroblasts), thereby expanding red blood cell (RBC) production. Meanwhile, in the liver, vadadustat increases production of transferrin, the plasma iron carrier, and decreases production of hepcidin, the negative regulator of ferroportin. Increased iron availability and its delivery by transferrin to marrow erythroblasts increases RBC size and hemoglobin content. Furthermore, in the marrow, vadadustat increases release of reticulocytes compared with ESA administration.
In addition, Vadadustat is well-tolerated in healthy volunteers and patients with chronic kidney disease. It increases reticulocytes, plasma EPO, and Hb levels in a dose-dependent manner.
Reference:
[1] Koury MJ, et al. Am J Hematol. 2022 Sep;97(9):1178-1188.
[2] Pergola PE, et al. Kidney Int. 2016 Nov;90(5):1115-1122.