In molecular biology, CD18 (integrin beta chain 2) is an integrin beta chain protein encoded by the human itgb2 gene. Specifically, the lack of CD18 expression can lead to adhesion defects of circulating white blood cells. This reduces the immune system’s ability to resist foreign invaders. Besides, integrin CD11b/CD18 (Mac-1; CR3; αMβ2) is a heterodimer of αM (CD11b) and β2 (CD18) subunits, which is essential for leukocyte adhesion and migration and immune function. Integrin CD11b/CD18 is a more restrictive antigen and is usually present in circulating leukocytes in an inactive configuration. Moreover, they are the key receptors that mediate leukocyte adhesion, cross endothelial migration, flow into the injured site. Furthermore, CD11b/CD18 is rapidly activated to mediate leukocyte adhesion, migration, and accumulation in inflammatory sites. Although it can block integrin-mediated leukocyte adhesion, it has limitations on human inflammatory diseases. Leukadherin-1 is a specific of the leukocyte surface integrin CD11b/CD18.
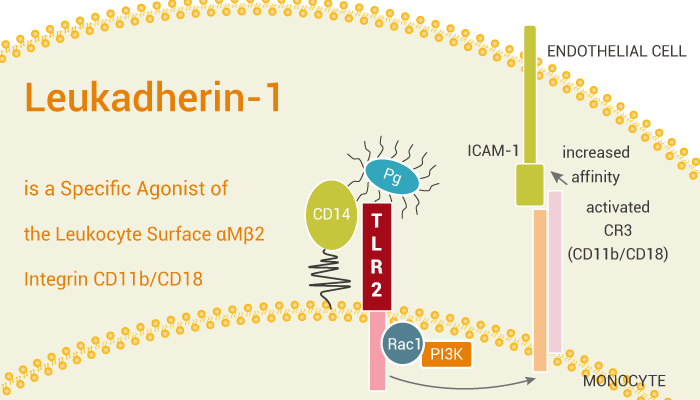
Leukadherin-1 is a specific agonist of the leukocyte surface αMβ2 integrin CD11b/CD18.
How does Leukadherin-1 work on the target? Let’s study it together. In the beginning, Leukadherin-1 increases CD11b/CD18-dependent cell adhesion to fibrinogen with an EC50 of 4 μM. Meanwhile, Leukadherin-1 enhances leukocyte adhesion to ligands (such as ICAM-1) and vascular endothelium. Thus Leukadherin-1 reduces leukocyte transendothelial migration and influx to the injury sites. Nonetheless, Leukadherin-1 suppresses innate inflammatory signaling.
In the second place, Leukadherin-1 pretreatment reduces the secretion of interferon (IFN)-γ, tumor necrosis factor (TNF), and macrophage inflammatory protein (MIP)-1β by monokine-stimulated NK cells. Particularly, Leukadherin-1 pretreatment also reduces the secretion of IL-1β, IL-6, and TNF by Toll-like receptor (TLR)-2 and TLR-7/8-stimulated monocytes.
Last but not the least, Leukadherin-1 with 1 mg/kg by i.p. twice daily for 14 days is beneficial in preventing hyperoxia-induced neonatal lung injury. Obviously, Leukadherin-1 improves alveolarization and vascular development. Additionally, Leukadherin-1 reduces pulmonary vascular remodeling and PH in a hyperoxia-induced experimental model of bronchopulmonary dysplasia (BPD).
All in all, Leukadherin-1 is a specific of the leukocyte surface αMβ2 integrin CD11b/CD18.
References:
Jagarapu J, et al. Am J Respir Cell Mol Biol. 2015;53(6):793-801.